7 Years - Partners Health Plan Gets Results
7 Years - Partners Health Plan Gets Results
Dear Members Families, & Friends,
We invite you to join us in celebrating PHP’s 7th Anniversary!
|
In 2016, we launched a non-profit organization and a new model of care for Individuals with Intellectual and Developmental Disabilities (IDD). We have delivered life-changing benefits and person-centered care coordination under a single and holistic plan. For the past seven years, we have been dedicated to improving lives. We are very proud of what we have done to make healthcare more accessible to reduce health disparities. Below are highlights from last year. Thank you for putting your trust in Partners Health Plan. We are grateful each and every day that we can assist members and families live their best lives! With Gratitude
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
What Did We Do in 2022?
We Excelled
-
An independent evaluation funded by the Centers for Medicare & Medicaid Services (CMS) reports that PHP’s innovative solutions like the pharmacy management program reduced errors, unnecessary emergency department visits, and length of hospital stays.
-
The telehealth program successfully resolved 90% of member’s concerns which prevented trips to the hospital.
-
More members completed colorectal cancer screening; diabetes testing and controls; controlled high blood pressure; completed annual dental visits and received annual flu vaccines compared to national and New York State health plans.
-
90% of PHP members have received at least one dose of the primary COVID-19 vaccination.
-
70% of the eligible members have received the booster dose.
We Talked About Diversity, Equity, & Inclusion
- We expanded the Diversity, Equity, & Inclusion (DEI) Department, added more staff volunteers to our dedicated DEI council with representation from across the organization, held multiple cultural recognition forums and safe space conversations, and added to our DEI related education modules for staff.
We Expanded Our Services & Supports
-
We added 1,200 new providers, including Stonybrook Medicine enhancing our Network for members on Long Island.
-
Implemented an in-house Patient Care Assessment team to quickly get home care services in place.
-
New contracts with DentaQuest & Ridehealth to provide better dental & transportation services.
-
Partnered with Solvere Health to pilot specialized IDD mobile dental clinics at select-day service locations in Metro New York.
-
Over-the Counter (OTC) cards were added to the benefit package for more than 600 community members.
-
We launched a text messaging program to provide health care reminders, supporting preventative health care and wellness for our members.
We Supported You
- Our Designated Representative Committee met 96 times to review more than 700 Life Plans.
-
PHP hosted 3 Member & Family meetings, 4 Participant Advisory Committee meetings, 6 family education sessions, and 8 Peer Empowerment Group meetings.
We Advocated
- Provided recommendations to OPWDD Commissioner Neifeld regarding COVID-19 protections for people with IDD.
- Members and families testified before the General Assembly on the 2023-2027 OPWDD 5.07 Strategic Plan.
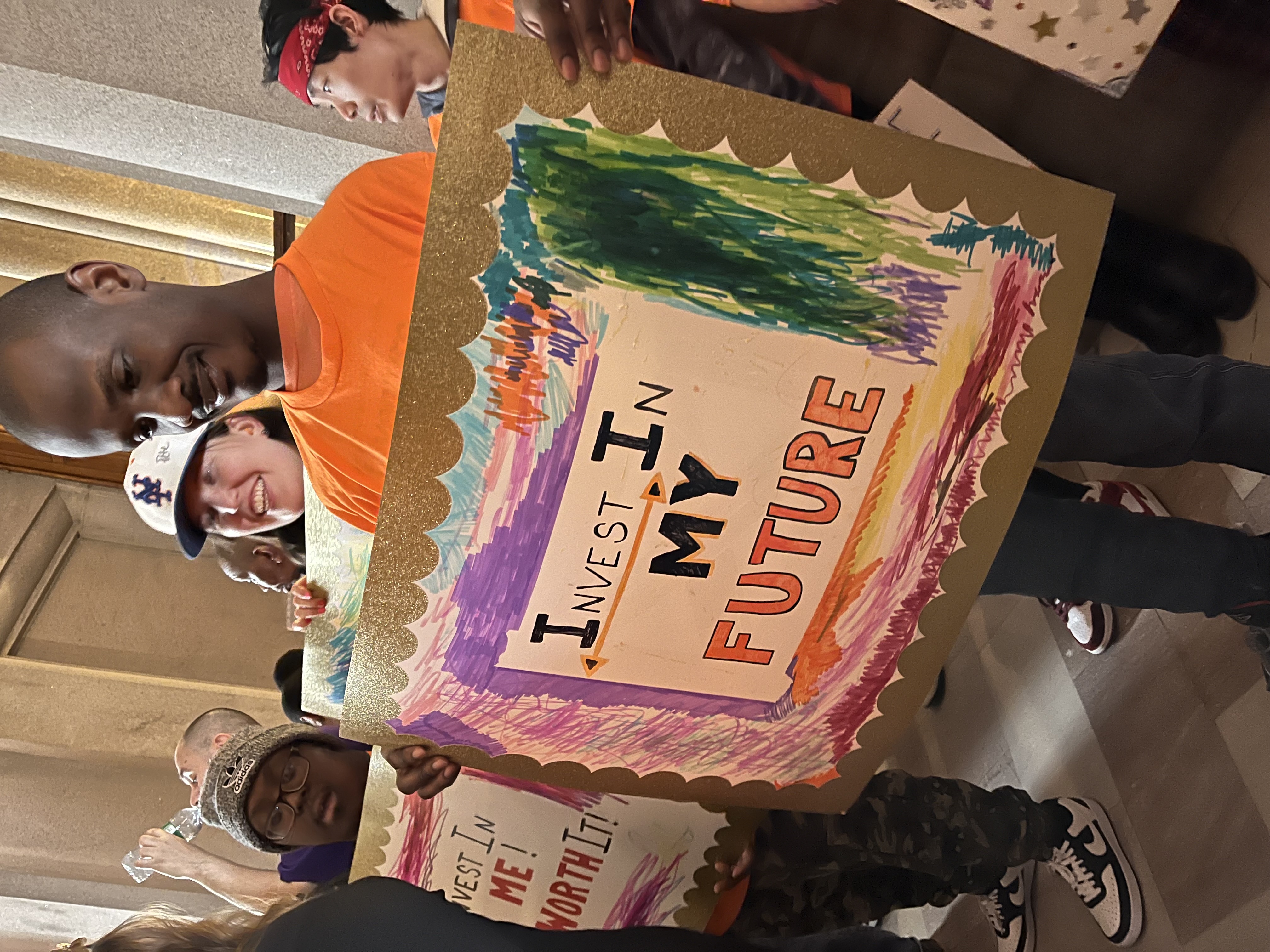
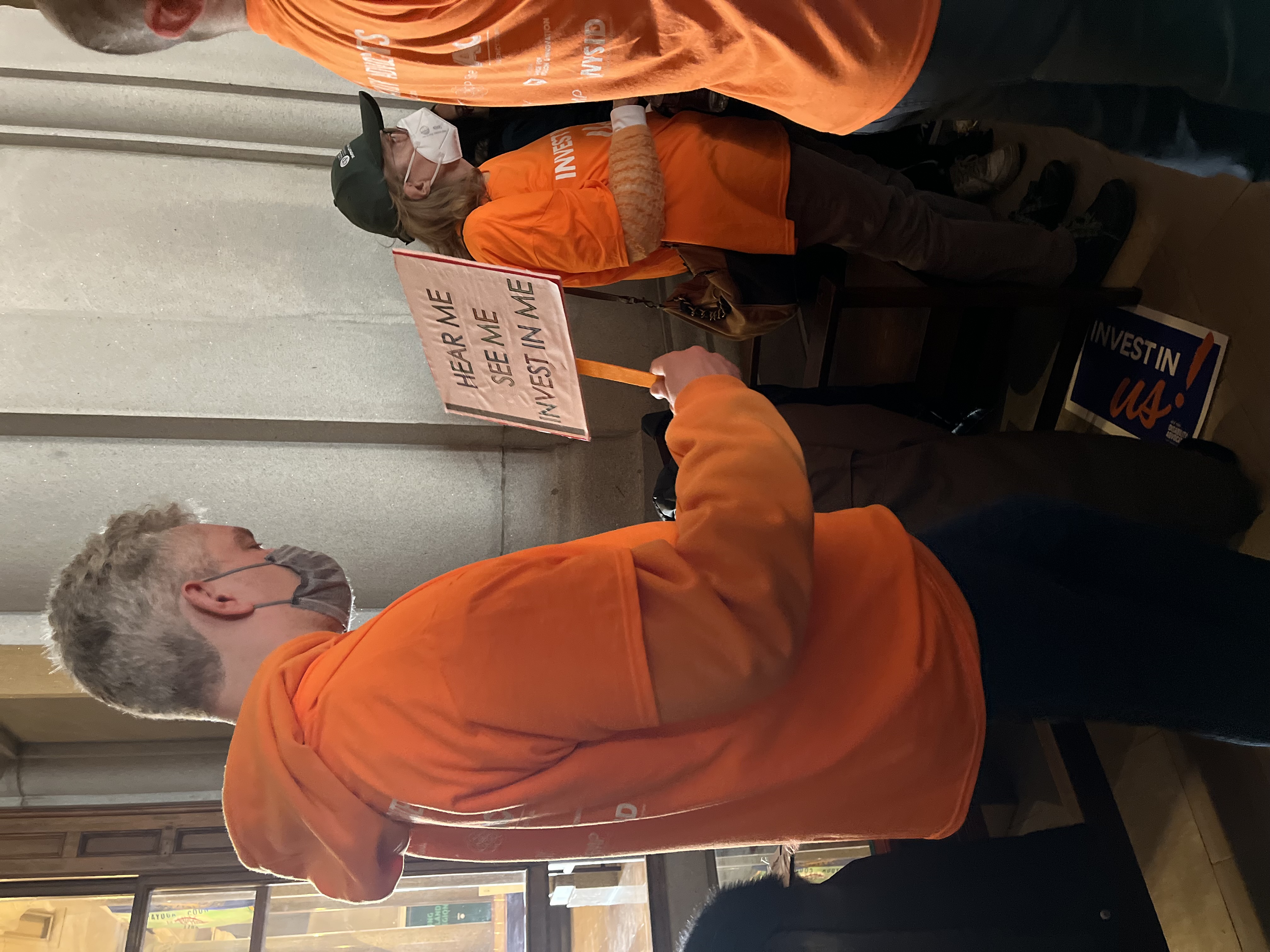
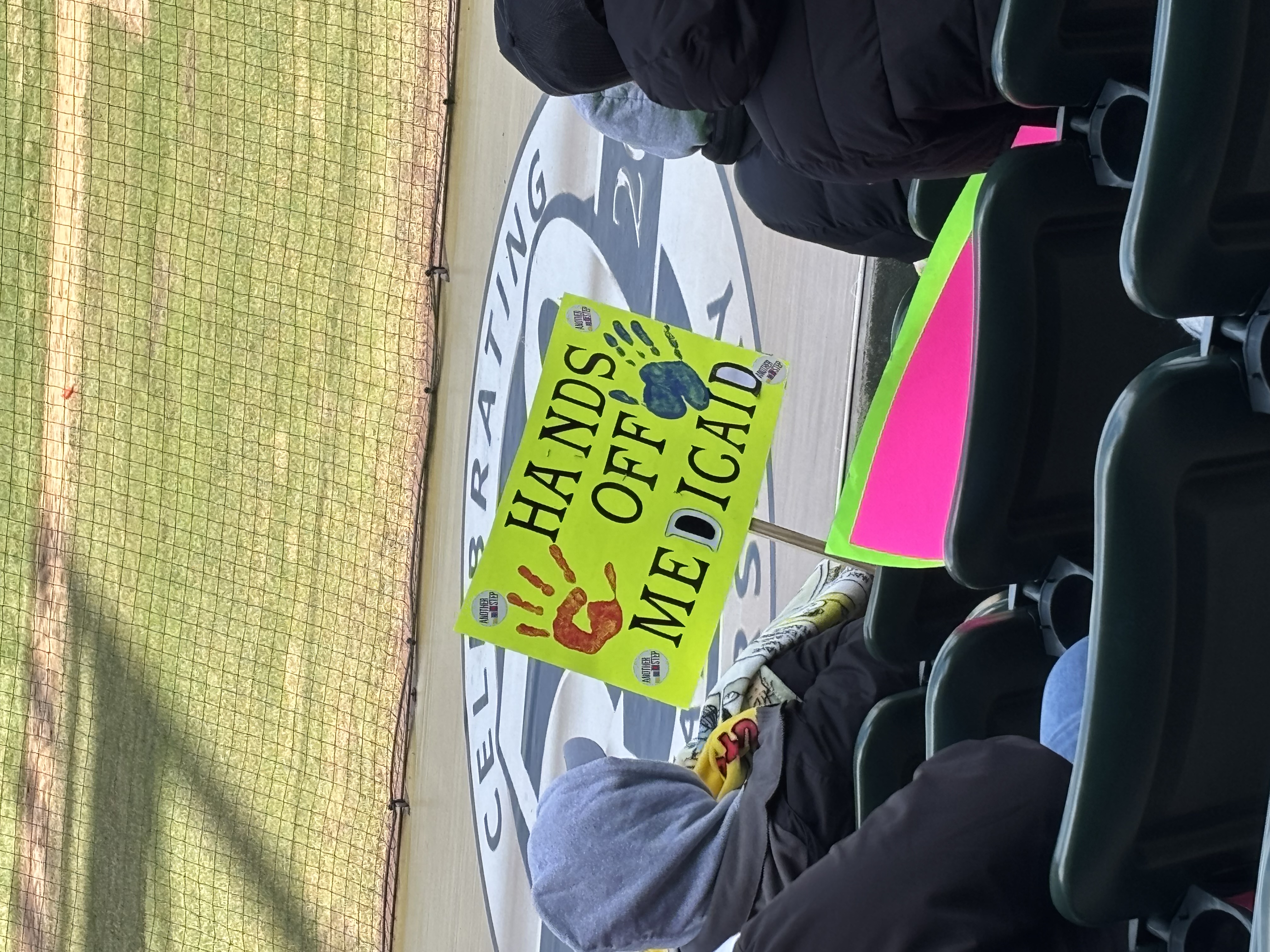
- Members, families, and staff rallied at the NYS Capitol in support of Direct Support Professionals (DSPs).
-
Comments provided by PHP resulted in modifications to the proposed DOH 1115 waiver changes.
We Celebrated
- PHP earned NCQA-Certification on the HEDIS Compliance Audit